Author: Belinda Dowsett, Associate Director, Medical Devices / IVD, PharmaLex Australia
Through continued increases in technological capabilities in material engineering, imaging and manufacturing, physicians are now in a position to provide medical devices specifically tailored to meet the needs of an individual patient. While this approach has been around for some time, particularly in the context of “custom-made devices” manufactured by medical device companies in appropriate facilities, more and more medical devices are being manufactured at the point of care. While this brings with it many advantages, it is also creating a challenge for global regulators who are grappling with the development of the regulatory framework to support such design and manufacturing operations.
Personalized Medical Devices
Patient-matched medical devices are only one type of medical device within this concept of “personalized medical devices”. It is also worth pointing out the other types of personalized medical devices within the global regulatory framework – custom-made devices, adaptable medical devices and medical device production systems.
- Custom-made devices are entirely unique and bespoke devices, made for one particular patient to meet their specific anatomical, physiological or pathological condition. It is very much one of a kind and is not simply an adjustment to an existing device.
- Adaptable medical devices are those specifically designed to be adapted, adjusted or shaped at the point of care to meet the patient needs.
- The medical device production system is a relatively new concept and it relates to a system of equipment, materials and tools specifically designed and intended to produce medical devices. The system is produced by a regulated manufacturer and is typically supplied to healthcare professionals for producing medical devices for their patients.
Point-of-Care Manufactured Devices
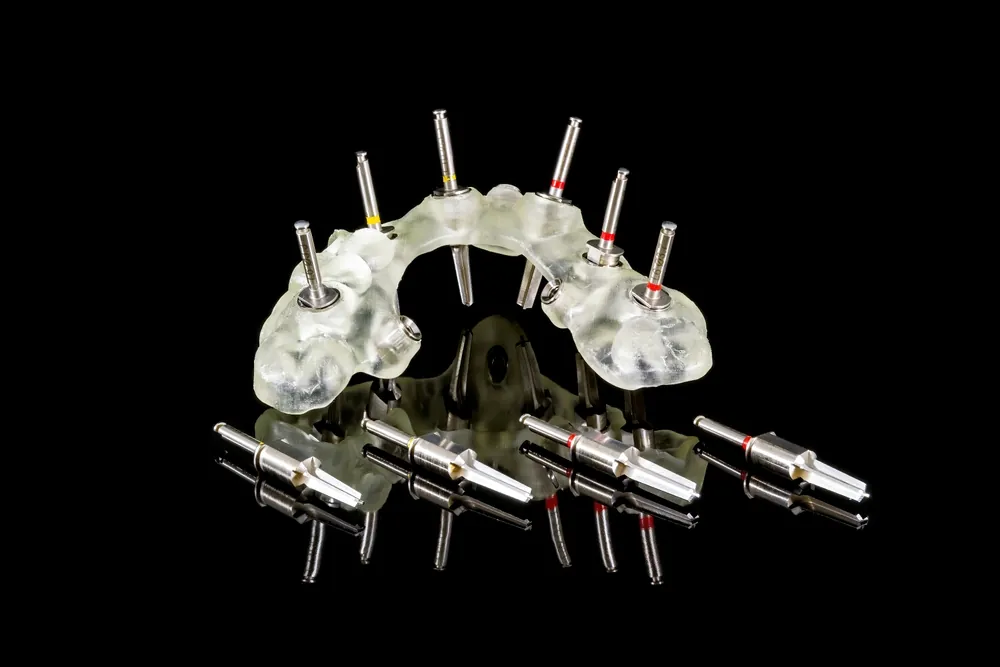
The scope of point-of-care manufactured devices is wide-ranging – from relatively simple dental aligners or patient anatomical models to more complex surgical guides and dental appliances. But what these types of devices have in common are the benefits their personalisation offers to the patient and the healthcare professionals.
The patient benefits include the ability to customise to a patient’s unique anatomical or physiological characteristics, to improve surgical or procedure outcomes and to reduce complications. Healthcare professionals can see benefits from improved surgical planning, decreased surgical risk and increased accuracy and precision.
Alongside all of this are the benefits afforded to industry. By providing a framework for the regulation of personalized medical devices, industry has the opportunity to provide medical device solutions that actually meet the individual needs of patients. It also allows close cooperation between physicians and other healthcare professionals to ultimately improve patient outcomes.
Global Regulatory Approach
For patient-matched medical devices, Europe, Australia and the US each have a framework that requires pre-market approval of the device’s design envelope and the approval is required under the responsibility of the legal manufacturer. Each regulator also has specific exemptions around the supply of custom devices.
The regulations differ around the considerations for point-of-care manufacturing or medical device production systems (MDPS).
In the US, the Food and Drug Administration (FDA) has been across this for some time, with guidance on additive manufactured medical devices being released in 2017 and product codes and regulations being available for both 3D printers and 3D printing materials such as resins. They are also currently working on a discussion paper for point-of-care manufacturing to drive the direction of future regulation in this space.
In Europe, there is nothing specifically defined within the European Union Medical Device Regulation (EU MDR) around point-of-care manufacturing. However, there are provisions for parts, components and materials intended to be used in personalized medical devices, to be placed on the market as medical devices according to the MDR, and be subject to the same controls and regulations as for any other medical device.
In Australia in February 2021 the personalized medical device framework was introduced. Included in these changes was the concept of the medical device production system (MDPS), however this has yet to be implemented and discussions with stakeholders will determine what this will ultimately look like.
The Challenge
The concept of personalized medical devices, and in particular point-of-care manufactured medical devices, is forcing regulators to reconsider their approach to regulation.
The idea of a device manufacturer is no longer limited to a certified manufacturing facility, but could also now include the doctors, dentists and allied health professionals working within their clinic or office. Not only are there limitations on the control of these facilities, but how does the regulator ensure the safety and performance of the device that has been produced? What level of documentation or evidence is required to be developed or maintained by the operator or clinician?
There is also a need to specifically define the level of control that manufacturers are required to demonstrate over medical device production systems and how this may be assessed by regulators.
Conclusion
Ultimately, regulators need to determine how they can best use the regulations to drive the safety and effectiveness of medical devices, particularly as it relates to patient-matched and point-of-care manufactured devices.
The current regulatory framework is not sufficient to account for all the variables and nuances associated with point-of-care medical device manufacturing. Through industry and stakeholder consultation we are expecting regulators to adapt their regulatory models to account for the expanding definition of “manufacturer” and consider options for oversight or certification of facilities and users.