Author: James Morrison
The human body’s biggest organ is the skin. It is also our best organ because it keeps the outside out and our insides in. Yet, despite its remarkable toughness and durability, it is still a living thing, regularly re-growing itself every 28 days, and needs to be protected from the harms it might suffer from medical devices.
In October 2020, US FDA issued a (draft) guidance, titled: Select Updates for Biocompatibility of Certain Devices in Contact with Intact Skin. The major point of this guidance is that manufacturers do not need to include biological test results when submitting their device for clearance to market, providing certain conditions are met. Now is a good time to reflect on that guidance, the limiting conditions, the science behind it, and how manufacturers should make the best use of it.
The guidance only applies to medical devices in direct contact with intact skin, regardless of the contact duration. All skin contact devices have the same “endpoints for biological evaluation” (harms) identified in ISO 10993-1, Table A.1, namely: Cytotoxicity, Sensitisation and Irritation. These are the harms considered by FDA in issuing this guidance.
Indirect skin-contact devices are mentioned but excluded from this guidance. In these devices, indirect contact is mediated through some fluid (in this case liquid) medium that transports leachable substances from the device to the intact skin.
It is interesting to note that the test methods for each of the listed harms (see ISO 10993-5, -10 and -23 respectively) include a method for the direct contact of the test article on the test system. Nonetheless, it is far more common to apply test methods that use extracts (polar & non-polar) of the test article. Extraction of the test article increases the sensitivity of the test system, by increasing the availability of leached substances. However, extraction is not a good representation of clinical reality of direct contact with intact skin. In clinical application, there is generally no liquid phase present to leach substances from the device. In some cases, there may be sweat present, but this is largely polar (thus non-polar extracts are not relevant) and would not be very common.
Further, this guidance only applies to medical devices composed of certain materials, including:
Synthetic Polymers:
- Acrylonitrile butadiene styrene (ABS);
- Cured epoxy adhesives;
- Fluoropolymers including polytetrafluoroethylene (PTFE), expanded polytetrafluoroethylene (ePTFE), polyvinylidene fluoride (PVDF), and fluorinated ethylene propylene (FEP);
- High impact polystyrene (HIPS);
- Polyamides, including nylon;
- Polybutylene terephthalate (PBT);
- Polycarbonate (PC);
- Polyetheretherketone (PEEK);
- Polyether imide (PEI);
- Polyethylenes, including low-density polyethylene (LDPE) and high-density polyethylene (HDPE);
- Polyethylene terephthalate (PET);
- Polymethylmethacrylate (PMMA);
- Polyoxymethylene (POM);
- Polyphenolsulfone (PPSU);
- Polypropylene (PP);
- Polyurethane (PU); or
- Silicone (elastomers)
Fabrics:
- Polyurethane fabrics, including Lycra;
- Cotton fabrics;
- Polyamide fabrics, including nylon; or
- Silk fabrics
There is also a list of six exclusions:
- Materials that are not listed above list, including novel materials and bulk metals;
- Devices stored in or containing fluids or creams;
- Device fabricated from in-situ polymerizing materials, absorbable materials, or hydrogels;
- Devices contacting breached or compromised skin;
- Reprocessed single-use devices; and
- Adhesives to attach a device directly to the skin.
Materials scientists will immediately observe that “synthetic polymers” are macro-molecules and have relatively low chemical reactivity compared to their size. Hence, they are often biologically “inert.” However, they are very rarely used in their pure form, and commercial resins always contain some minor additions, including antioxidants, UV stabilisers and other functional additives. Such additives may have a somewhat higher potential for (biological) reactivity than the base polymer, but they are present in relatively low concentrations and are typically selected for their stability and compatibility with the polymer. There is a relatively low risk of such additives migrating out of the finished item. This makes FDA feel somewhat comfortable about their use under somewhat less stringent conditions.
A notable polymer missing from the list is PolyVinyl Chloride (PVC). There may be more than one reason for this, but two reasons spring to mind immediately: a) the Vinyl Chloride monomer is toxic at relatively low doses, and b) the polymer is often highly plasticized, (up to 60% plasticizer), which tends to migrate out. Ortho-phthalate plasticisers, historically very common but now being phased out in manufactured product, are endocrine disruptors. The identification and use of all manner of plasticisers in PVC are very good grounds for its exclusion from the list.
Other readers may also have noticed that the fabrics list does not include polyester, a very common garment fibre; however, PET, the base polymer from which almost all polyester fibres are made, is included in the polymer list. Polyesters for fibres are made by the mega-tonne and are not always well controlled in terms of composition. The increasing use of recycled/post-consumer resources in the fabric fibre industry also adds to uncertainty about composition. Also, as polyester fibre is very easy to dye, there are very many dye chemistries available to the industry, again of varying control and indeed toxicity. Therefore, it is reasonable that polyesters as fabrics are not included.
The question of dyeing fabrics also leads to a question about colouring medical devices, including coloured plastics. FDA considers coloured medical devices to be “adulterated.” There are quite strict FDA controls around (quite a small list of permissible) colourants, but FDA is yet to publish any biocompatibility guidance on this subject.
Dyeing of the natural fibres generally uses dyes that are of similar toxicity to the substrate or are very strongly bonded and therefore not chemically available. Synthetic fibres pose other problems. Polyamides are very hard to dye, so the dyes are strongly chemically bonded. Polyurethanes like elastane/Lycra are impossible to dye, so pigments are compounded in before spinning. Polyesters can be dyed with a vast array of dye chemistries (of varying toxicities.) Such matters are important for medical device fabrics because the colourants/dyes are bonded to the fibre surface, and the real surface area of a fabric is orders of magnitude greater than the apparent surface area.
Manufacturers of medical devices incorporating fabrics should be well aware of, and therefore very cautious about, the considerable complexity of the fabric finishing processes, particularly the plethora of obtuse chemical residues on the fabric. Dyeing fabrics is a bit of an obscure “art.” A thorough understanding of the manufacturing/finishing process, including modification if necessary, is highly recommended.
Colouring plastic components used in medical devices is generally done by dispersing the colourant through the material during the conversion into the (moulded/extruded) item. Because the colourants are distributed (evenly) throughout the volume of material, the availability at/to the surface is relatively low (“to” the surface, because particles can migrate and molecules can be leached.) Consequently, colourants from plastic mouldings and similar, have relatively low biological risk.
Manufacturers can then, in place of biological testing, use other technical/administrative control measures to satisfy the FDA concerning the safety of their skin contact devices. There are three key pieces of information required:
- Clear and concise description/definition of all materials used to fabricate the device with direct or indirect skin contact;
- Confirmation that those materials have a documented history of safe use in legally US-marketed medical devices in contact with intact skin; and
- Confirmation that the device is not excluded.
These requirements are to ensure the FDA that the manufacturer has control of the composition of their device, has adequately evaluated it for biological safety, and is in conformity with this guidance. Within this draft guidance, there is also a helpful list of six quality system requirements and post-market controls that can be invoked to give substance to the submission.
Overall, this particular guidance document is very helpful in terms of expressing requirements, so manufacturers can have confidence in using it somewhat as a template to ensure that their biological evaluations and documentation meets the agency’s expectations.
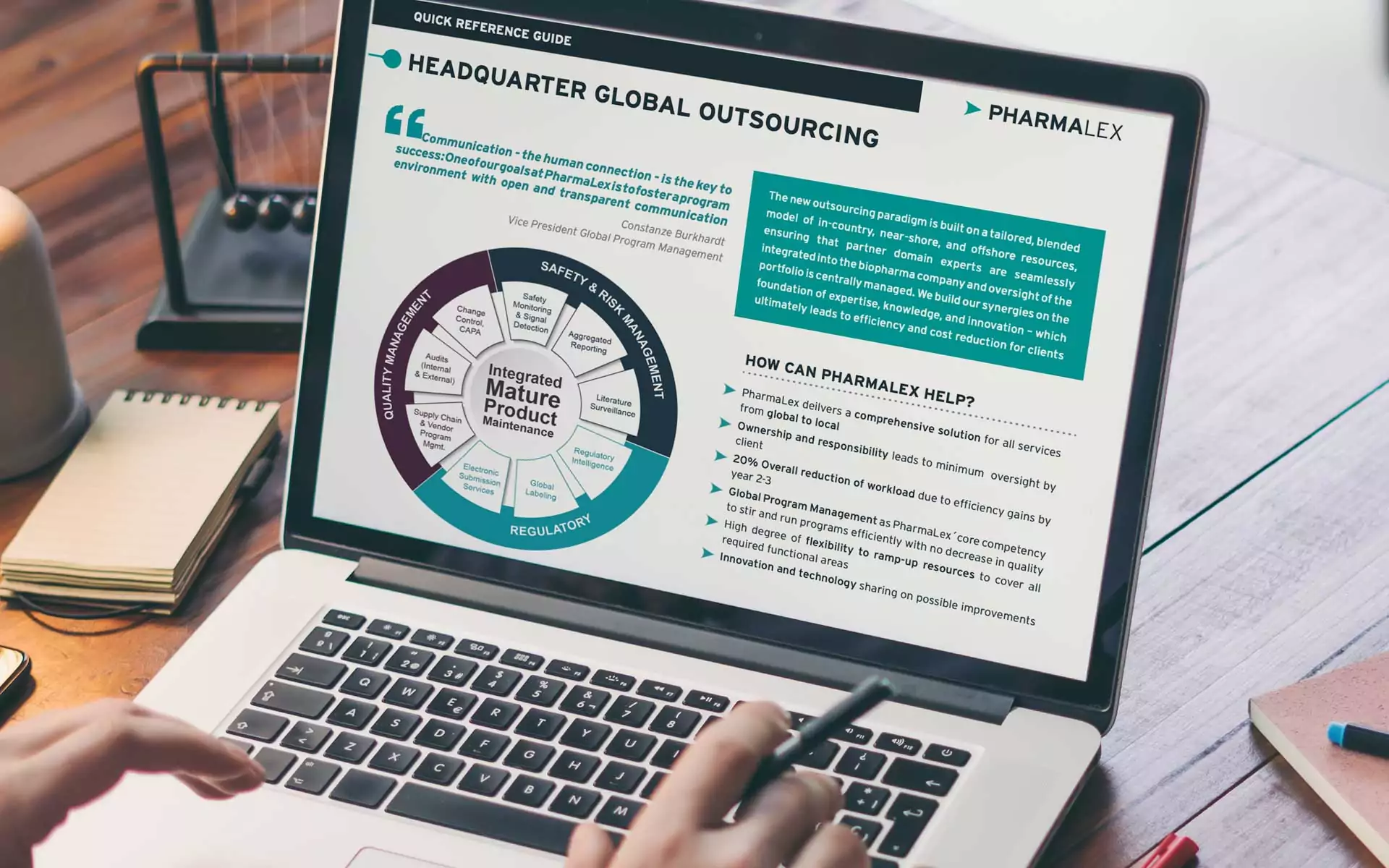
As always manufacturers may find managing these matters, and complying with guidance, to be a challenge. PharmaLex experts are always available to assist in all levels of medical device safety and compliance. Please feel free to reach out to us for guidance and assistance in this matter.Contact us